Author: Dr. Deniz KATIRCIOGLU ÖZTÜRK, Group Manager – Healthcare Programs
While AI recently acts as a “silver surfer” in the hype cycles, IoT stands as its closest buddy all along its entourage. Almost every smart and connected mechanism, now, claims to bear the humble crown of an IoT item. Since “health” and “well-being” are among the top priorities in our lives, it was inevitable that we would pay special attention to healthcare IoT devices and study them under a new subtitle, Io(M)T, where “M” obviously stands for “Medical”.
Io(M)T is basically a herd of connected medical devices that have adopted all aspects of the IoT way of technology as well as the solutions to challenging safety and data security issues. As posh as it sounds, can we say Io(M)T is on par with general IoT in terms of market and technology potential ? Indeed, it seems likely since the market is predicted to reach hundreds of billions of dollars worldwide by 2021
Although the general IoT market effectively targets the “layman”, Io(M)T holds value over gross-niche market full of people with much higher “willingness to pay”. But this “willingness” is not in vain, for sure. Expectations are high for the fundamentals such as safety and security of data generated and processed by Io(M)T, in exchange for the money paid. While maintaining the connectivity, the risk of compromising sensitive medical data is straight out higher than that of a general-purpose IoT device. As the repercussions of a possible leakage or malfunction increase, likely legal recourse of Io(M)T users appear on the horizon of higher legislative ranks and Io(M)T manufacturers.
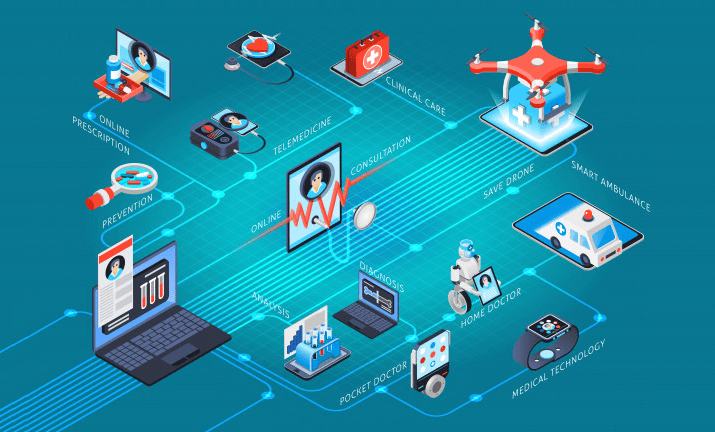
Just like the majority of the IoT devices, many Io(M)T instances now oscillate between two modus operandi of “full” and “reduced” functionalities while being administered to our bodies through wearable, digestible and implantable interfaces. The full mode (FFD) – with relatively little concern about resources – satisfies the data hunger of smart algorithms, while the reduced mode (RFD) acts in the minimal protocol set with a lower power consumption.
Starting with the big players such as legacy imaging devices in a healthcare facility, many more have been recently added to the range of Io(M)T devices (e.g. infusion pumps, implantable cardiac devices, smart insulin pens, thermometers and temperature sensors, vital monitors, connected inhalers, ingestible medication sensors, coagulation testers, intelligent hearing aid appliances, smart bras for breast cancer detection, wireless pill bottles, hand hygiene monitors, smart soles with GPS, smart watches for major depressive disorder, robotics surgery, connected hospital beds, smart urinary catheters, “location-as-a-service” elder trackers, transdermal drug delivery patches, so on and so forth).
With this versatility and its operational space covering the whole human body, Io(M)T proudly deserves a new moniker, IoB, short for “Internet of Bodies”. Especially, during the recent pandemic days, the significance of remote monitoring and data sampling being “human independent” came to the fore. In the most widely observed model, the IoB’s “point-of-care pipeline” starts with the digital capture of data from the intended part of the body. Then, the data is relayed to a remote observation or a smart assessment interface that feeds analysis and vigilance mechanisms. As might be envisioned, operational possibilities are fanning-out from every hop along this pipeline. Though potentially promising, these can bring many risks and implicit challenges, too. It should not be forgotten even for a moment that IoB is an approach that builds its predicates on the measurables of human body and health. As a natural consequence of this, privacy issues blended with legal and ethical hurdles raise a red flag from the opposite corner.
The Health Insurance Portability and Accountability Act (HIPAA), defining a set of regulations for the health data emerging with conventional methods, is quite successful as an addressee of these particular issues [5]. The incorporated law explicitly holds accountable the domain actors like healthcare service providers and facilities, insurance companies and the business associates handling sensitive data. Nonetheless, no explicit rule, regulation or law has yet been devised to protect the indirect information and knowledge obtained from the “captured data” using tools of analytics and AI.
Apparently, IoB is the right medium for the myosis of sensitive data and paves the way for the cross-over to produce “offspring information” that is yet to be labelled as “sensitive”. Gradually, the processes of drawing inferences regarding personal health, therapeutical pathways, insurance profiling and precision strategies over billing reimbursement have already started to use the so-called deduced information due to lack of appropriate legal shield protecting that information. The points where these types of information are transmitted and the junctions where they are used are increasing at an exponential pace. Prophesized it is that humanity, who is either currently unaware or uncomplaining about this surveillance capacity, may face some form of discrimination or unfair treatment based on information collected and produced through digital means.
Yes, IoB helps advance patient engagement; yes, it ensures the delivery of evidence-based care; yes, it monitors the service quality; yes, it aids timely intervention; and yes, it provides data that helps generate novel hypotheses. However, its holistic and connected surveillance trait might arouse a social response among the conscious and hyper-vigilant population, just like the “London Surveillance Experiment”. In the meantime, technology evangelists have a negligent bias regarding the subject of “mass surveillance”. Non-technical and non-medical topics such as personal rights, private life, behavioral and environmental conditions are swallowed like a “side dish” by the computational appetite fueled by data diversity and opportunities promised by IoB. Alas, personal privacy concerns accompanying the IoB will be a tough nut to crack for the foreseeable future.
[ 1 ] Sharma, N., Shamkuwar, M., & Singh, I. (2019). The history, present and future with IoT. In Internet of Things and Big Data Analytics for Smart Generation(pp. 27-51). Springer, Cham.
[ 2 ] Mahajan, S. (2020). IoT In Healthcare Market Size, Growth and Industry Trends Report, 2026.
[ 3 ] Aksu, H., Babun, L., Conti, M., Tolomei, G., & Uluagac, A. S. (2018). Advertising in the iot era: Vision and challenges. IEEE Communications Magazine, 56(11), 138-144.
[ 4 ] Jawhar, I., Mohamed, N., & Agrawal, D. P. (2016). A hierarchical wireless sensor network design for monitoring a pipeline infrastructure. In Industrial Wireless Sensor Networks(pp. 189-211). Woodhead Publishing.
[ 5 ] Cohen, I. G., & Mello, M. M. (2018). HIPAA and protecting health information in the 21st century. Jama, 320(3), 231-232.